Aptean Insights
Whether you’re looking for industry insights, product details, upcoming events or our latest news it’s all right here. Browse the categories below or get in touch with one of our experts if you have a question.
Results
Showing1-15of1935
 Podcast Dec 22, 2025ERP Perspectives: Dynamic Production and Active IngredientsLearn how supplement and cosmetic manufacturers manage ingredient potency variation and maintain batch-to-batch consistency using ERP tools designed for dynamic formulation control.
Podcast Dec 22, 2025ERP Perspectives: Dynamic Production and Active IngredientsLearn how supplement and cosmetic manufacturers manage ingredient potency variation and maintain batch-to-batch consistency using ERP tools designed for dynamic formulation control.Listen now
 Blog Post Dec 19, 2025Ensuring Batch-to-Batch Consistency: Tackling Ingredient Potency Variation in Supplements and CosmeticsLearn how to manage ingredient potency variation and achieve batch-to-batch-consistency in supplements and cosmetics with a life sciences ERP system.
Blog Post Dec 19, 2025Ensuring Batch-to-Batch Consistency: Tackling Ingredient Potency Variation in Supplements and CosmeticsLearn how to manage ingredient potency variation and achieve batch-to-batch-consistency in supplements and cosmetics with a life sciences ERP system.Learn More
 Press Release Dec 18, 2025Aptean and CAS Expand Collaboration with Biosequence Chemical Modifications SolutionAptean and CAS expand their collaboration with a new biosequence chemical modifications solution to accelerate life science patent search and analysis.
Press Release Dec 18, 2025Aptean and CAS Expand Collaboration with Biosequence Chemical Modifications SolutionAptean and CAS expand their collaboration with a new biosequence chemical modifications solution to accelerate life science patent search and analysis.Read more
 Blog Post Dec 17, 2025Turning AI Anxiety Into Advantage: A Leaders Guide to the Future of AI in BusinessGrowth requires courage. Discover how to overcome hesitation and use AI to drive lasting business success with advice from Aptean CEO, TVN.
Blog Post Dec 17, 2025Turning AI Anxiety Into Advantage: A Leaders Guide to the Future of AI in BusinessGrowth requires courage. Discover how to overcome hesitation and use AI to drive lasting business success with advice from Aptean CEO, TVN.Learn More
 Product Tour Dec 16, 2025Aptean Life Sciences ERP: Dynamic Production FunctionalitySee how Aptean's life sciences ERP dynamically scales production ingredients based on variable potencies in this demo.
Product Tour Dec 16, 2025Aptean Life Sciences ERP: Dynamic Production FunctionalitySee how Aptean's life sciences ERP dynamically scales production ingredients based on variable potencies in this demo.Watch
 Blog Post Dec 12, 2025Apparel ERP Benefits in Action: Customer Success Stories and TestimonialsDiscover how apparel businesses are transforming operations with an ERP built for the industry. Explore real customer success stories and testimonials showcasing improved efficiency, accuracy, and growth.
Blog Post Dec 12, 2025Apparel ERP Benefits in Action: Customer Success Stories and TestimonialsDiscover how apparel businesses are transforming operations with an ERP built for the industry. Explore real customer success stories and testimonials showcasing improved efficiency, accuracy, and growth.Learn More
 Press Release Dec 11, 2025Logility is recognized in the 2025 Gartner® Voice of the Customer for Supply Chain Planning SolutionsLogility achieved a 4.9/5 rating and 100% Willingness to Recommend in the 2025 Gartner® Voice of the Customer for Supply Chain Planning Solutions.
Press Release Dec 11, 2025Logility is recognized in the 2025 Gartner® Voice of the Customer for Supply Chain Planning SolutionsLogility achieved a 4.9/5 rating and 100% Willingness to Recommend in the 2025 Gartner® Voice of the Customer for Supply Chain Planning Solutions.Read more
 Datasheet Dec 10, 2025Aptean Transportation Management System (TMS) for Apparel WholesalersDiscover how Aptean’s Transportation Management System helps apparel wholesalers streamline logistics, reduce shipping costs, and improve delivery efficiency with smarter, automated workflows.
Datasheet Dec 10, 2025Aptean Transportation Management System (TMS) for Apparel WholesalersDiscover how Aptean’s Transportation Management System helps apparel wholesalers streamline logistics, reduce shipping costs, and improve delivery efficiency with smarter, automated workflows.Download
 eBook Dec 9, 2025The Algorithm: AI from Concept to Competitive AdvantageDownload Edition 2 of The Algorithm to see how AI is becoming a true differentiator, with insights on agentic AI, expert perspectives, and real-world adoption from brands like Aviva.
eBook Dec 9, 2025The Algorithm: AI from Concept to Competitive AdvantageDownload Edition 2 of The Algorithm to see how AI is becoming a true differentiator, with insights on agentic AI, expert perspectives, and real-world adoption from brands like Aviva.Download
 Datasheet Dec 3, 2025Aptean Food & Beverage ERP FoundationAptean Food & Beverage ERP Foundation offering provides a simplified, economical deployment tailored for small and midsize businesses, ensuring a smooth and efficient implementation without sacrificing quality.
Datasheet Dec 3, 2025Aptean Food & Beverage ERP FoundationAptean Food & Beverage ERP Foundation offering provides a simplified, economical deployment tailored for small and midsize businesses, ensuring a smooth and efficient implementation without sacrificing quality.Download
 Success Story Nov 27, 2025Tecumseh Tunes Up Tech Stack With Aptean TMSDiscover how Tecumseh streamlined operations and boosted efficiency by implementing Aptean TMS. See the impact of smarter logistics technology on performance.
Success Story Nov 27, 2025Tecumseh Tunes Up Tech Stack With Aptean TMSDiscover how Tecumseh streamlined operations and boosted efficiency by implementing Aptean TMS. See the impact of smarter logistics technology on performance.Download
 Blog Post Nov 26, 2025Real Route Planning Software Benefits According to the Businesses That Use ItDiscover real route planning software benefits—cost savings, efficiency gains and on-time delivery—straight from the companies using Aptean Routing & Scheduling.
Blog Post Nov 26, 2025Real Route Planning Software Benefits According to the Businesses That Use ItDiscover real route planning software benefits—cost savings, efficiency gains and on-time delivery—straight from the companies using Aptean Routing & Scheduling.Learn More
 Product Tour Nov 24, 2025See Our Shop Floor Control Software In ActionExplore how our shop floor control software unifies operator activity, performance monitoring and production visibility in one easy-to-use platform.
Product Tour Nov 24, 2025See Our Shop Floor Control Software In ActionExplore how our shop floor control software unifies operator activity, performance monitoring and production visibility in one easy-to-use platform.Start My Product Tour
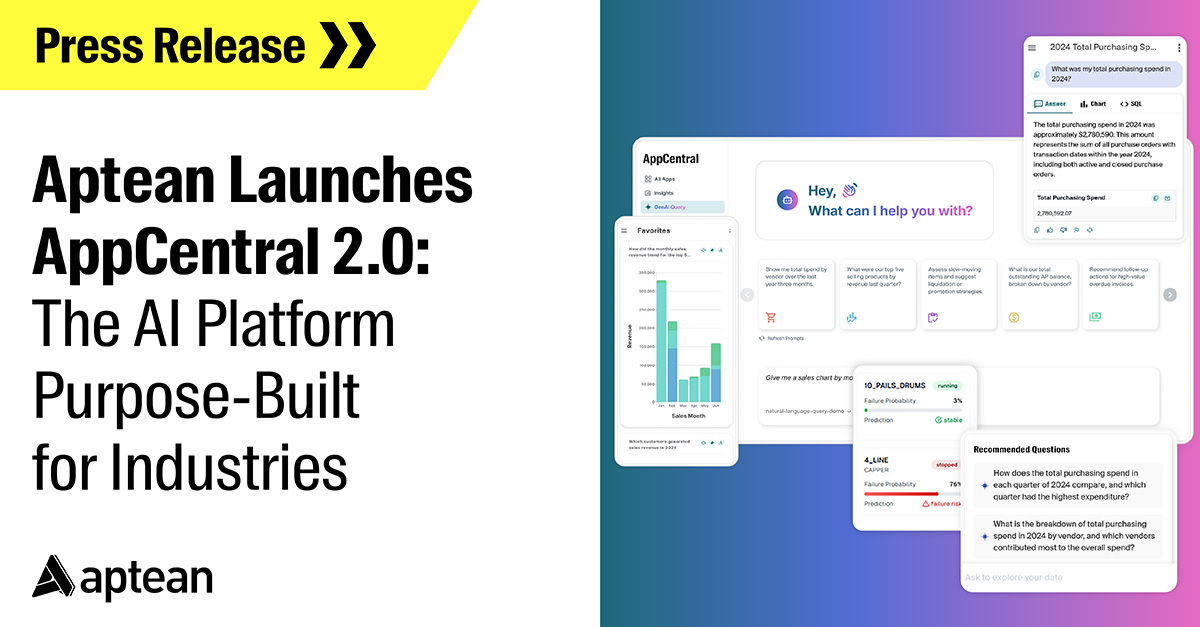 Press Release Nov 20, 2025Aptean Launches AppCentral 2.0: The AI Platform Purpose-Built for IndustriesAptean unveils AppCentral 2.0, an AI platform for industries that drives smarter decisions, faster operations, and real-time business agility.
Press Release Nov 20, 2025Aptean Launches AppCentral 2.0: The AI Platform Purpose-Built for IndustriesAptean unveils AppCentral 2.0, an AI platform for industries that drives smarter decisions, faster operations, and real-time business agility.Read more
 eBook Nov 20, 2025Your Discrete Manufacturing Solutions Buyer's GuideExplore the essential features, benefits and key considerations for choosing the right discrete manufacturing software. Get the insights you need to make a confident, informed decision.
eBook Nov 20, 2025Your Discrete Manufacturing Solutions Buyer's GuideExplore the essential features, benefits and key considerations for choosing the right discrete manufacturing software. Get the insights you need to make a confident, informed decision.Download
Ready To Start Transforming Your Business?
We’ve got the specialized industry software to help your organization thrive.