Aptean Insights
Whether you’re looking for industry insights, product details, upcoming events or our latest news it’s all right here. Browse the categories below or get in touch with one of our experts if you have a question.
Results
Showing1-15of1951
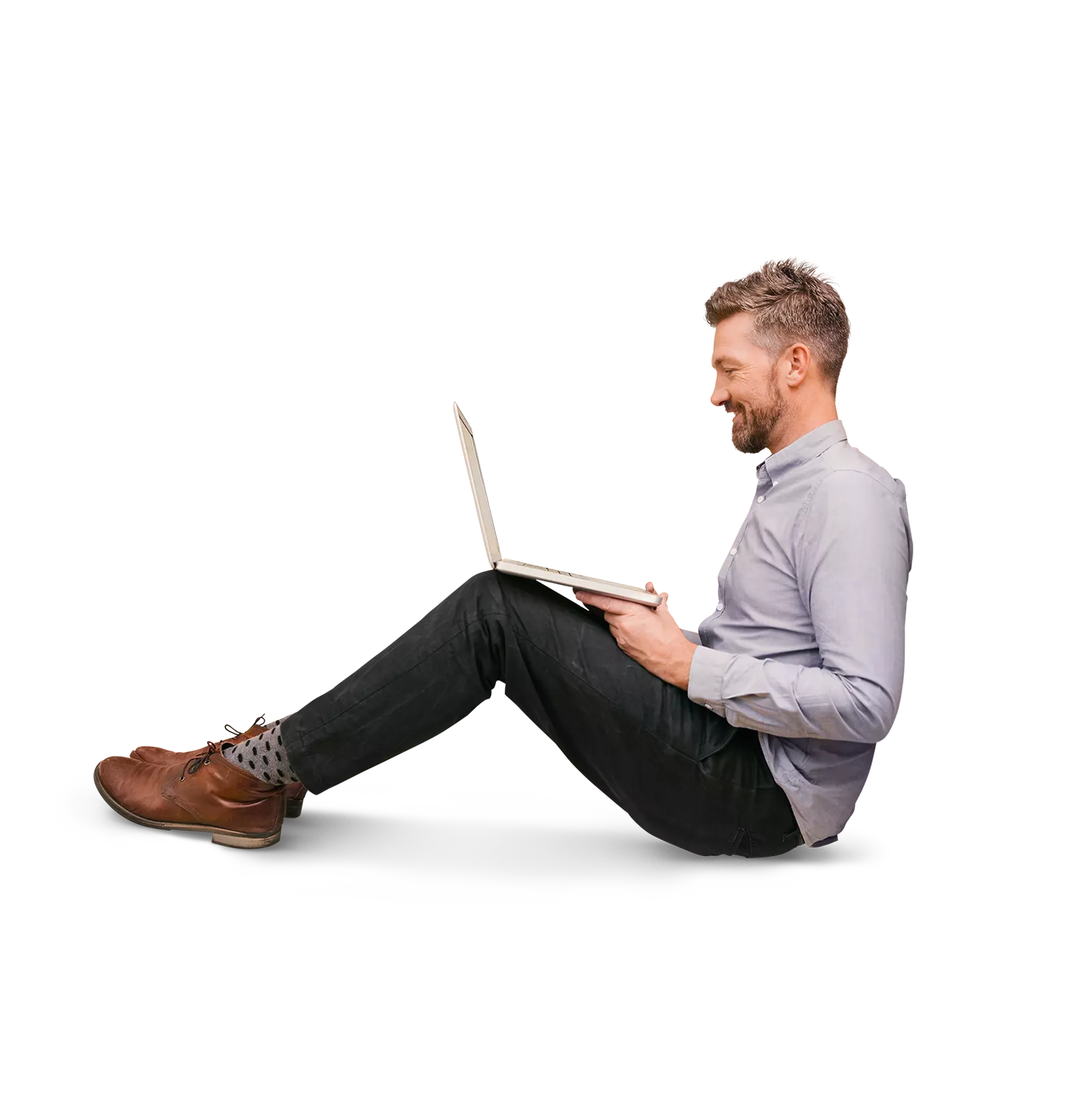
 Datasheet Jan 27, 2026Aptean Industrial Manufacturing ERP Intuitive Edition on AppCentralAptean Industrial Manufacturing ERP, Intuitive Edition gives discrete manufacturers greater visibility into all areas of their business. Click here to learn more, now.
Datasheet Jan 27, 2026Aptean Industrial Manufacturing ERP Intuitive Edition on AppCentralAptean Industrial Manufacturing ERP, Intuitive Edition gives discrete manufacturers greater visibility into all areas of their business. Click here to learn more, now.Download
 Datasheet Jan 26, 2026Aptean Industrial Manufacturing ERP Made2Manage Edition on AppCentralIf you want to streamline your operations, reduce costs and improve your supply chain visibility, Aptean Industrial Manufacturing ERP, Made2Manage Edition is right for your business.
Datasheet Jan 26, 2026Aptean Industrial Manufacturing ERP Made2Manage Edition on AppCentralIf you want to streamline your operations, reduce costs and improve your supply chain visibility, Aptean Industrial Manufacturing ERP, Made2Manage Edition is right for your business.Download
 Whitepaper Jan 26, 2026Equipment ERP Implementation Best Practices: A Guide to SuccessFrom the pre-implementation phase to post-implementation, this guide explores equipment ERP implementation best practices to help ensure a seamless and successful software deployment.
Whitepaper Jan 26, 2026Equipment ERP Implementation Best Practices: A Guide to SuccessFrom the pre-implementation phase to post-implementation, this guide explores equipment ERP implementation best practices to help ensure a seamless and successful software deployment.Download
 Blog Post Jan 21, 2026The Business Benefits of Discrete Manufacturing ERP: Real Results from Aptean CustomersDiscover real-world discrete manufacturing ERP case studies showing higher output, faster growth and better visibility with Aptean.
Blog Post Jan 21, 2026The Business Benefits of Discrete Manufacturing ERP: Real Results from Aptean CustomersDiscover real-world discrete manufacturing ERP case studies showing higher output, faster growth and better visibility with Aptean.Learn More
 Press Release Jan 16, 2026Aptean Acquires OpsVeda to Bring End-to-End Agentic Orchestration to the Logility Supply Chain Planning and Execution PlatformSee how Aptean’s AI solutions with OpsVeda and Logility empower supply chain leaders to eliminate blind spots and drive execution with real-time intelligence.
Press Release Jan 16, 2026Aptean Acquires OpsVeda to Bring End-to-End Agentic Orchestration to the Logility Supply Chain Planning and Execution PlatformSee how Aptean’s AI solutions with OpsVeda and Logility empower supply chain leaders to eliminate blind spots and drive execution with real-time intelligence.Read more
 Blog Post Jan 14, 2026The 2026 AI Business Trends You Need To KnowAI is moving from hype to execution. Explore the key AI business trends shaping 2026—and what leaders must do to stay ahead.
Blog Post Jan 14, 2026The 2026 AI Business Trends You Need To KnowAI is moving from hype to execution. Explore the key AI business trends shaping 2026—and what leaders must do to stay ahead.Learn More
 Feb32026Event / WebinarEveryday GenAI | Free AI and AppCentral LearningFeb 3, 2026 OnlineExplore free AI and AppCentral learning with step-by-step tutorials, courses, and resources to automate tasks, streamline workflows, and unlock GenAI queries for everyday answers and faster success.
Feb32026Event / WebinarEveryday GenAI | Free AI and AppCentral LearningFeb 3, 2026 OnlineExplore free AI and AppCentral learning with step-by-step tutorials, courses, and resources to automate tasks, streamline workflows, and unlock GenAI queries for everyday answers and faster success.Register Now
 Press Release Jan 12, 2026Aptean and CAS Expand Collaboration with Biosequence Chemical Modifications SolutionDiscover how Aptean and CAS are expanding their collaboration with a biosequence chemical modifications solution. Get inspired by what’s next
Press Release Jan 12, 2026Aptean and CAS Expand Collaboration with Biosequence Chemical Modifications SolutionDiscover how Aptean and CAS are expanding their collaboration with a biosequence chemical modifications solution. Get inspired by what’s nextRead more
 Feb52026Event / WebinarFrom Craft to Cohesion: How Chelten House Modernized Operations Without Compromising QualityFeb 5, 2026 OnlineDiscover how Chelten House modernized its operations without compromising quality, achieving greater efficiency, visibility, and cohesion while staying true to its craft.
Feb52026Event / WebinarFrom Craft to Cohesion: How Chelten House Modernized Operations Without Compromising QualityFeb 5, 2026 OnlineDiscover how Chelten House modernized its operations without compromising quality, achieving greater efficiency, visibility, and cohesion while staying true to its craft.Register Now
 Feb92026Event / WebinarVisit Aptean Supply ChainFeb 9, 2026 Las Vegas, NVLearn how Aptean Supply Chain helps businesses streamline operations, enhance visibility, and drive smarter supply chain decisions.
Feb92026Event / WebinarVisit Aptean Supply ChainFeb 9, 2026 Las Vegas, NVLearn how Aptean Supply Chain helps businesses streamline operations, enhance visibility, and drive smarter supply chain decisions.Discover More
 Feb262026Event / WebinarMove beyond dashboards. Learn how GenAI orchestrates logistics decisions and execution in real time.Feb 26, 2026 OnlineDiscover how GenAI moves logistics beyond dashboards to orchestrate real-time decisions and execution across operations.
Feb262026Event / WebinarMove beyond dashboards. Learn how GenAI orchestrates logistics decisions and execution in real time.Feb 26, 2026 OnlineDiscover how GenAI moves logistics beyond dashboards to orchestrate real-time decisions and execution across operations.Register Now
 Mar32026Event / WebinarVisit Aptean at Natural Products Expo WestMar 3, 2026 Natural Products Expo West in AnaheimMeet Aptean at Natural Products Expo West in Anaheim. Visit Booth #3199C for live demos of our new AI-powered AppCentral for Food & Beverage platform and connect with our team to discuss your growth plans.
Mar32026Event / WebinarVisit Aptean at Natural Products Expo WestMar 3, 2026 Natural Products Expo West in AnaheimMeet Aptean at Natural Products Expo West in Anaheim. Visit Booth #3199C for live demos of our new AI-powered AppCentral for Food & Beverage platform and connect with our team to discuss your growth plans.Discover More
 Mar32026Event / WebinarPredict to Perform | Free AI and AppCentral LearningMar 3, 2026 OnlineJoin Predict to Perform for free AI and AppCentral learning through live and on-demand sessions designed for real-world impact.
Mar32026Event / WebinarPredict to Perform | Free AI and AppCentral LearningMar 3, 2026 OnlineJoin Predict to Perform for free AI and AppCentral learning through live and on-demand sessions designed for real-world impact.Register Now
 Mar172026Event / WebinarReady for Intelligent Action | Free AI and AppCentral LearningMar 17, 2026 OnlineBuild practical AI skills and transform insight into action with Ready for Intelligent Action, offering free AI and AppCentral learning.
Mar172026Event / WebinarReady for Intelligent Action | Free AI and AppCentral LearningMar 17, 2026 OnlineBuild practical AI skills and transform insight into action with Ready for Intelligent Action, offering free AI and AppCentral learning.Register Now
 Podcast Dec 22, 2025ERP Perspectives: Dynamic Production and Active IngredientsLearn how supplement and cosmetic manufacturers manage ingredient potency variation and maintain batch-to-batch consistency using ERP tools designed for dynamic formulation control.
Podcast Dec 22, 2025ERP Perspectives: Dynamic Production and Active IngredientsLearn how supplement and cosmetic manufacturers manage ingredient potency variation and maintain batch-to-batch consistency using ERP tools designed for dynamic formulation control.Listen now
Ready To Start Transforming Your Business?
We’ve got the specialized industry software to help your organization thrive.